Exploring Nutrition and Well-Being in Older Adults
As people age, their nutritional needs change significantly, and ensuring proper nutrition becomes essential for maintaining health, preventing chronic diseases, and successfully promoting overall well-being. Older adults face unique challenges that can affect their dietary habits and nutritional status, including changes in metabolism, appetite, and physical abilities. The following in-depth article explores the critical role of nutrition in the well-being of older adults, the specific nutritional needs of this population, common challenges they face, and strategies to promote healthy eating as part of an overall comprehensive approach to aging well.
The Importance of Nutrition
Good nutrition is fundamental to health at every stage of life, but it becomes increasingly important as people age. The right nutrition can help to prevent or manage chronic conditions. These conditions include heart disease, diabetes, osteoporosis, and cognitive decline. It also plays an incredibly vital role in maintaining muscle mass, bone density, and overall physical and mental well-being.
As the body ages, it undergoes various physiological changes that can impact nutritional needs:
- Decreased Metabolic Rate: As people age, their basal metabolic rate decreases, meaning they require fewer calories to maintain their body weight. However, the need for essential nutrients doesn’t decrease, and in some cases, it may increase. This creates a need for a nutrient-dense diet that provides adequate nutrition without excessive calories.
- Changes in Body Composition: Aging is often associated with muscle mass loss (sarcopenia) and an increase in body fat. This shift in body composition can affect mobility, strength, and overall health. Adequate protein intake and physical activity are critical for maintaining muscle mass and preventing frailty.
- Altered Digestive Function: Aging can affect the digestive system, leading to reduced absorption of certain nutrients such as vitamin B12, calcium, and iron. These changes may require adjustments in diet or the introduction of supplements to ensure sufficient nutrient intake.
- Changes in Appetite and Thirst: Many older adults experience a decrease in appetite and thirst. This can lead to inadequate food and fluid intake. Factors such as medications, chronic illnesses, and changes in taste and smell can also cause a reduced food intake.
- Increased Risk of Chronic Diseases: Older adults are more likely to develop chronic conditions such as cardiovascular disease, diabetes, and osteoporosis. Nutrition plays a huge role in the prevention and management of these diseases, highlighting the importance of a balanced, nutrient-rich diet.

Specific Nutritional Needs of Older Adults
Older adults have specific nutritional requirements that differ from those of younger people. Meeting these needs is essential for maintaining health and quality of life. The following nutrients are particularly important for older adults:
- Protein: Protein is essential for maintaining muscle mass, repairing tissues, and supporting immune function. Seniors may need more protein than younger adults to counteract the effects of sarcopenia. High-quality protein includes lean meat, poultry, fish, eggs, dairy products, legumes, and plant-based proteins like tofu and quinoa.
- Calcium and Vitamin D: These are crucial for bone health. Older adults and seniors are at increased risk of osteoporosis and fractures, making an adequate intake of these nutrients essential. Dairy products, fortified foods, leafy greens, and fish such as salmon are good sources of calcium. Vitamin D can be acquired from sunlight exposure, fortified foods, and supplements if necessary.
- Fiber: A high-fiber diet promotes digestive health, helps to prevent constipation, and can reduce the risk of heart disease and diabetes. Whole grains, fruit, vegetables, legumes, and nuts are excellent sources of dietary fiber. Older adults should aim for at least 25–30 grams of fiber per day.
- B Vitamins: B vitamins, particularly B12 and folate, are important for brain health, red blood cell production, and DNA synthesis. Older adults may have difficulty absorbing B12 from food, so fortified foods or supplements may be necessary. Good sources of B vitamins include leafy greens, whole grains, eggs, meat, and fortified cereals.
- Omega-3 Fatty Acids: Omega-3 fatty acids, found in fatty fish such as salmon, mackerel, and sardines, as well as in flaxseeds and walnuts, are important for heart health and cognitive function. These healthy fats have anti-inflammatory properties and can help to reduce the risk of heart disease and cognitive decline.
- Antioxidants: Vitamins C and E, beta-carotene, and selenium help to protect cells from any damage caused by oxidative stress. A diet that features a lot of colorful fruit and vegetables, nuts, seeds, and whole grains provides a variety of antioxidants that support healthy aging.
- Hydration: The right fluid intake is essential for maintaining overall health. Dehydration is a common concern among older adults, as the sensation of thirst diminishes with age. It’s important for older adults to drink a good amount of water and consume fluids throughout the day, including hydrating foods like fruit and vegetables.
Common Nutritional Challenges for Older Adults
While the nutritional needs of older adults are well understood, meeting these needs can be challenging due to a variety of factors. Understanding these challenges is key to developing effective strategies for improving nutrition in the elderly population.
- Reduced Appetite: As mentioned earlier, many older adults experience a decrease in appetite due to factors such as changes in taste and smell, medications, and chronic health conditions. This can lead to inadequate nutrient intake and unintentional weight loss.
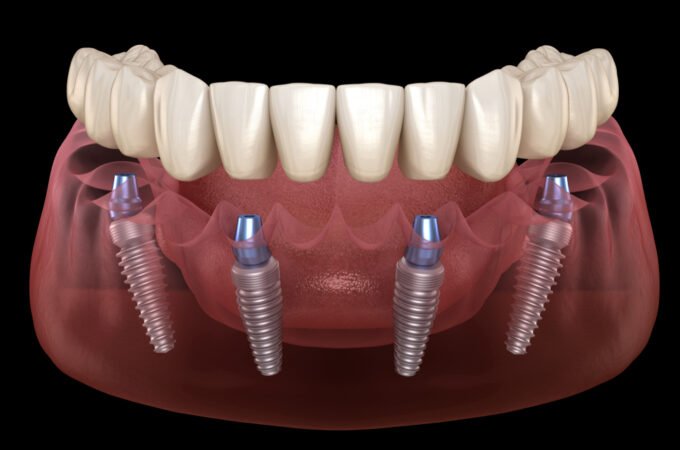
- Difficulty Eating and Swallowing: Dental issues, such as missing teeth or poorly fitting dentures, can and will make chewing difficult. Conditions like dysphagia (difficulty swallowing) are also common among older adults, leading to a preference for softer, less nutrient-dense foods.
- Social Isolation: Eating is often a social activity, and older adults who live alone may be less motivated to prepare and eat balanced meals. Social isolation can lead to poor dietary habits, such as skipping meals or relying on convenience foods that are low in nutrients. Moving into a care home can help older adults to combat feelings of isolation as many have dedicated eating areas where residents can sit together. St Peters is one of the leading care homes in Bury St Edmunds that offers community living so loneliness and isolation is successfully overcome.
- Limited Mobility: Physical limitations can make grocery shopping, meal preparation, and even eating more difficult. Older adults with limited mobility may have difficulty accessing fresh, healthy foods and may rely on processed or pre-packaged meals that are often high in sodium, unhealthy fats, and sugar.
- Financial Constraints: Many older adults live on fixed incomes, which can make it challenging to afford nutritious foods. Financial limitations may lead to a reliance on cheaper, less nutritious options, further compromising dietary quality.
- Chronic Health Conditions: Chronic illnesses such as diabetes, heart disease, and kidney disease can require special dietary considerations, adding complexity to meal planning and making it more difficult to meet nutritional needs.
- Medication Interactions: Certain medications can affect appetite, nutrient absorption, and metabolism. For example, some medications may interfere with the absorption of vitamins and minerals, while others may cause side effects such as nausea or dry mouth that reduce food intake.

Strategies to Promote Healthy Nutrition in Older Adults
Addressing the nutritional challenges faced by older adults requires a multi-faceted approach that considers their physical, social, and economic circumstances. Here are some key strategies to promote healthy eating and well-being in older adults:
- Personalized Meal Planning: Tailoring meal plans to the individual’s preferences, dietary needs, and physical abilities is crucial. For those with a reduced appetite, offering smaller, nutrient-dense meals more frequently throughout the day can help to ensure adequate nutrition. Including favorite foods and flavors can also make meals more appealing.
- Nutrient-Dense Foods: Encourage the consumption of nutrient-dense foods that provide essential vitamins and minerals without excessive calories. Foods such as fruit, vegetables, whole grains, lean proteins, and low-fat dairy should be prioritized. Smoothies, soups, and stews can be nutritious and easier to consume for those with dental issues or swallowing difficulties.
- Supplements When Necessary: While food should be the primary source of nutrients, supplements may be necessary for older adults who have difficulty meeting their nutritional needs through diet alone. Vitamin D, calcium, and B12 are common supplements for older adults, but supplementation should always be guided by a healthcare professional.
- Social Support: Combat social isolation by encouraging older adults to eat meals with family, friends, or in community settings. Group meals, senior centers, and social programs can provide opportunities for social interaction and improve motivation to eat.
- Accessible and Convenient Food Options: For those with limited mobility, consider options like grocery delivery services, meal delivery programs, or the use of adaptive kitchen tools to make meal preparation easier. Providing easy-to-prepare, healthy snacks and meals can help to ensure that nutrition is maintained even when cooking is a challenge.
- Education and Awareness: Educating older adults and their caregivers about the importance of nutrition and how to make healthy food choices is essential. Providing information on how to read food labels, plan balanced meals, and manage special dietary needs can empower older adults to take charge of their nutrition.
- Addressing Financial Barriers: Connecting older adults with resources such as food assistance programs (e.g., SNAP, Meals on Wheels) can help to alleviate financial constraints and ensure access to nutritious foods. Community programs that provide free or low-cost meals are also valuable resources.
- Monitoring and Support: Regular monitoring of nutritional status by healthcare providers is important for identifying and addressing potential issues early on. This includes tracking weight, assessing dietary intake, and checking for signs of malnutrition or nutrient deficiencies. Involving dietitians and nutritionists in the care of older adults can provide specialized guidance and support.
Final Thoughts
Nutrition plays a fundamental role in the well-being of older adults, influencing their physical health, cognitive function, and overall quality of life. As people age, their nutritional needs change, and addressing these needs requires a comprehensive, individualized approach.
By understanding the specific nutritional challenges faced by older adults and implementing strategies to promote healthy eating, we can support healthier, more fulfilling lives for our aging population. Holistic care that integrates nutrition with physical, social, and emotional support is essential for ensuring that older adults thrive in their later years.